



Research Article - (2023) Volume 12, Issue 1
Background: Migrants like African American(AA) and Caribbean population in High Income Countries (HIC)have been assessed as being at higher risk for late screening for Human Immune Deficiency Virus (HIV), a disease which can be prevented by adapting necessary safe sexual measures and giving Anti-Retroviral Therapy (ART) in initial stages. Timely diagnosis and treatment initiation plays significant role in optimizing HIV related health outcomes and lower transmission rates. This review aimed to evaluate and assess the effectiveness of different interventions conducted to increase the uptake of HIV testing in our targeted population.
Method: Ovid Medline, Embase, and Central Cochrane were searched on 2 July 2021 and potentially relevant studies identified were undertaken for reference screening. We considered Randomized Controlled Trials (RCTs) and studies conducted after 2008 with interventions to increase HIV testing uptake in AA and Caribbean population in HIC. Screening, data extraction and critical appraisal was conducted by one reviewer.
Finding: In our review 9 studies met the inclusion criteria. Six various types of interventions were identified conducted in different settings and targeting sub-population like MSM, Transgender and women from AA population. Majority interventions applied behaviour change models and targeted migrants from different ethnicities like Latino, Mexican, Asian and AA population.
Interpretation: Trials implementing multilevel interventions at AA churches and peer/health worker supported interventions through social networking recruitment, prevailed over structural and cultural barriers to show moderate effect estimate. Blending Provider Initiated Testing And Counseling (PITC) with existing primary healthcare settings looks promising and would encourage HIV testing uptake through patient-doctor/health worker relationships among migrant populations.
Universal health coverage; Health spending; Health insurance; Out-of-pocket payment
Nigeria HIV is a viral infection attacking immune system of the body causing various vulnerable infections more likely Acquired Immunodeficiency Syndrome (AIDS), which is not a treatable disease and is transmissible through different routes [1]. Delayed HIV diagnosis is associated with negative health outcomes like higher chances of hospitalization , reduced life expectancy by 10 years and ten-fold increased risk of death [2]. Highly sensitive, specific diagnostics and progressive rapid tests with fast results and early treatment have the potential to reach maximum population due to its easy adaptability and thus prevent immune deterioration and transmission of HIV, ART given in time reduces viral load majorly and thus reduces transfer rate and mortality and morbidity, in diagnosed individuals [3, 4]
In HICs like United States of America (USA), Canada, and Australia, sexual route is the most common route of transmission as due to proper screening procedures, blood/blood product related transmissions have been nearly abolished and inducing ART has decreased mother-to-child transmission drastically [5]. Research reveals that international migrants from high HIV prevalent countries as generalised epidemics, are contributing as larger number of HIV population in these HICs in contrast to their own citizens [6]. In many HICs unequal distribution of burden of HIV in most vulnerable populationlike immigrants, minor ethnicities like black Africans and Caribbean population are observed as the main reason for high HIV prevalence in HICs [7].
By 2018,USA had 1.2 million people with HIV, out of which 482900 were among Black African population living there, They accounted for 13% of the USA population but contribute as 42% (16,002) of 37,968 newly diagnosed HIV cases in USA and surrounding areas [8].
In 2015, WHO European region had 37% of newly detected HIV cases from migrants of the HIV cases transmitted by heterosexual contact and 37% were from sub-Saharan African countries [9]. These migrants are identified as the second largest group affected by HIV in European Union. Population at high risk of HIV are recommended an annual testing by Centres for Disease Control and Prevention, but 40% of AA are reported to be never tested. Statistics reveal that there were considerable disparities in subpopulations encountering delayed HIV diagnosis rates like in US the black African men report to have highest rates (65%).
Literature review indicates persistent effects of mistreatment and challenges faced due to cultural, social, structural, economical barriers and segregation at multilevel causing inequalities in accessing healthcare services in their receiving countries. The Legality and administrative actions expected to be faced by HIV positive individual and the stigma and discrimination associated not only adds on to the challenges but also discourages migrants to access HIV-related services, including testing and use of preventive measures. Addressing these barriers is crucial to pave a way for all HIV prevention efforts. Adaptation of rapid testing programmes and screening at primary care can possibly increase the HIV testing uptake in high-risk migrant populations and have a clear public health benefit.
To our knowledge there is not much conclusive information on interventions that could attain our objective, so this review was conducted to identify and assess interventions that focused to raise uptake of HIV testing in Black African and Caribbean migrant population in the various settings of HICs.
To assess effectiveness of interventions to increase the uptake of HIV screening by black African and Caribbean heritage communities in High Income Countries
Eligibility criteria
We included Studies meeting following inclusion criteria:
• Conducted after 2008 as the WHO and UNAIDS issued new guidelines encouraging “providerinitiated” HIV testing in healthcare settings. The objective was to widen HIV status awareness and increase access to HIV testing, treatment and prevention broadly.
• Conducted in HIC where a high-income economy is defined by the World Bank as a “Nation with a gross national income per capita of US$12,696 or more in 2020, calculated using the Atlas Method”.
• Only Randomized Controlled Trials (RCTs) as they are considered to be gold standard for evidence of effectiveness of interventions.
The participants population are black African/Caribbean heritage population living in HIC. Interventions to increase the uptake of HIV screening compared with the usual practice or any other comparative intervention were considered.
All the studies with outcome as HIV testing uptake as primary or secondary outcome and studies specifying population as AA/ Caribbean as a part of study population with results mentioned explicitly for them were included. We included English published studies due to lack of translation resources.
Set of Subject Headings were developed and relevant evidence were collected from Ovid Medline/ Embase collectively and Central Cochrane separately. Search Strategy was determined through consultation with an academic information specialist Miss Sarah Herring. RCT Filter was run at the end of the search. Search Strategy is presented in Appendix 1. Potentially relevant studies were included obtained through reference screening of, included studies and relevant ongoing trials and studies completed with no results posted. Due to limited time and lack of manpower other additional sources were not screened.
Preoperative marking was done while the patient in a standing position with a typical wise pattern skin incision. The Midline was marked from the manubrium sterni to the umbilicus, then marking the mid-axis of each breast from the middle point of the clavicle to the areola. Measuring the distance of the new Nipple Areola Complex (NAC) transposition, the new nipple-areola complex position tagged at Pitanguy point.
Dissection of the subcutaneous pocket superior to the new nipple areola complex position, with a distance equal to or more than the required distance of the nipple transposition. The pedicle base was not detached from the posterior region of the pectoralis fascia.
The technique is carried out by first, the areola is marked using the cookie cutter and incised, and depithelialization of the keyhole skin pattern is done using Colorado needle. Then, the breast tissue is excised only caudal to transverse limbs of the pillars down to but not breaching the pectoral fascia. 2 cm thick pillars are dissected medially, laterally. Superiorly, 0.5 cm-1 cm skin flap is adopted freeing the entire central breast mound. Thelength of superior/cephalic dissection is equal to the distance needed for NAC superior mobilization. The cephalic pocket must provide an ample room to accommodate the breast tissue to slide with minimal tension.
The constructed central mound is now freely mobile to slide up. Fixation of the central mound upper pole dermis to pectoralis fascia or at the second intercostal space with an absorbable suture 3/0 Monocryl at 9 o’clock, 12 o’clock and 3 o’clock. Finally, meticulous hemostasis, drains were never used. Once upper pole is fixed, then pillars are wrapped around the central mound and secured using stay stitch to the crossing of the breast meridian with IMF.
Closure is started caudal to cephalic. Initially, closure starts in the horizontal limb from periphery towards centre to enhance the breast perkiness and eliminate dog ears. Usually starting lateral first, done in layers. First layer using barbed suture to block the dead space and prevent the breast falling laterally. Second layer is a dermal layer, followed by the skin layer. Similar way of closure is done medially apart from the first layer “barbed suture layer” which is omitted medially to give more room for the breast to shift medially. Lateral side contour adjustment by liposuction was infrequently used.
Handling of citations
References identified from databases were further assessed in Endnote X9. References were de-duplicated and studies were imported to Rayyan software for abstract screening. Rayyan identified further duplicates. Titles and abstracts screening was run by single reviewer (due to non-availability of second reviewer) and references not meeting the inclusion criteria were excluded during this preliminary screening phase. Any doubts were discussed with supervisors and agreements reached.Full text copies were obtained through endnote and screened in detail to meet the inclusion criteria. A summary table of all excluded studies along with its reason for exclusion was provided. Standardised data extraction forms were used which were piloted on excel and adapted as necessary while extracting data. Data like objective of study, location, recruitment setting, sample size/type, participant characteristics, interventions, comparators, outcomes were extracted into the spreadsheet.
Data was extracted on the treatment effect estimates, odds ratio, percentage p-values, and confidence intervals. Cochrane Risk of Bias tool was used to appraise the methodological quality of the trials (ROB 2.0.). This includes domains covering the randomisation process, deviations from the intended intervention, missing outcome data, and measurement of the outcome. ROB assessment was used to assess the quality of quantitative data retrieved. The assessment was a part of the data extraction process
Synthesis
Summary of study characteristics was presented in data extraction for data synthesis. Trial data identified too heterogeneous to pool, or reported in a format not suitable for pooling, was presented as a narrative synthesis. It consisted of descriptive text and usage of various tables to summarise data to enable the reader to understand outcomes in the light of different interventions and recruitment process and identified potential bias for each study in the review. Process involved meticulously arranging studies by related population or outcomes assessed, summarising the results of the studies, summarising the range and size of the associations these reported by them, and detailing the most relevant study characteristics. A detailed commentary on the major methodological problems or biases that affected the studies were mentioned, together with a description of how this has affected the individual study results.
Meta-analysis methods
Identical interventions and settings studies were identified and summary measures of effect were estimated through formal meta-analysis. Dichotomous data was dealt by calculating the Relative Risk (RR)/Odds Ratio (OR) for each trial with the associated 95% Confidence Intervals (CIs). In multi-arm studies, independent comparison of each intervention arm with the control group was done.
Fixed effect model was used to calculate risks ratio, confidence interval and I2 and q statistics. We used Forest plots for visual assessment of heterogeneity and used the I2 and Q statistics measures. A Comprehensive plan for analysis was constructed before conducting it. Stata/IC 16.1 was used for performing Statistical analyses.
AA churches based multilevel intervention and religiously tailored intervention
Two RCTs conducted in AA churches with similar interventions given as multilevel HIV education were combined for metanalysis. Derose’16 recruited 5 churches with Latinos and AA as church members. It implemented multilevel intervention with HIV education workshops designed to raise awareness about HIV prevention and testing, peer leader workshops and HIV sermon/imagined contact scenario where each pastor or priest was asked to deliver a sermon about HIV and Congregation-based HIV testing events. Counselors conducted rapid oral fluid testing and counseling through a mobile clinic stationed at the church during regularly scheduled service. AA Baptist intervention churches showed higher rates of HIV testing during the follow-up compared to paired control churches (32% vs. 13%) with R.R of 2.48(C.I=1.50-4.18). Berkley 2020 recruited 4 AA churches with 543 AA adults as participants. It used religiously tailored multilevel intervention where individual-interpersonal contact, ministry groups educational games, printed/video testimonials, facilitated discussion, church services (sermons, responsive readings, church bulletins, church HIV stigma video, pastor-modeled receipt) and community outreach ministries. There was 23% increase in uptake of HIV testing seen in intervention group and 9% in control group. These two church-based interventions seem to have shown effect on increase in uptake of HIV testing. The meta-analysis done shows risk ratio as 1.94 (C.I-1.50-2.52)suggesting that the intervention group has 1.94 times chances of increase in uptake of HIV testing than the comparator group with I2 as 43.2% showing moderate heterogeneity.
Peer/Community Health worker(CHW) supported HIV education intervention:
peer support were grouped for metanalysis. Harawa, et al 2020 recruited 80 MSM from Public venues, community based organizations, parks, and events, provider referrals/fliers placed at public venues, online via Craigslist.com, Instagram, and a study website. He introduced Customized wellness peer supported plan that included referral to health and support services, incentives, peer encouragement, navigation and social education vs non peer supported control arm. Findings obtained are O.R=1.53 [0.21-11.03] showing moderate effect and R.R 1.12(C.I=0.91-1.38)
Kenya 2016 recruited 60 Adult AA from Over town neighborhoods of Miami by canvassing community centers, churches, and various community locations known as high traffic areas for our target population in the community. Intervention arm was given CHW assistance to complete homebased HIV rapid test (HBRHT, Ora Quick HIV test) and control arm was given no CHW assistance. All 30 participants in the intervention arm completed the HIV test and 27 participants from control arm completed the test with risk ratio as 1.10(C.I =0.97-1.25)
Study by Young 18 suggested that a peer-led HIV-testing intervention using social networking communities like paid social networking sites with targeted banner ads such as Facebook led to high rates of participant engagement and an increase in home-based HIV testing. The trial recruited 112 MSM. It used Peer leaders in 4 intervention group instructed to communicate about HIV prevention and testing compared to control group with Peer leaders communicating the importance of exercising, healthy eating, and maintaining a low-stress lifestyle. 44% participants from experimental group requested home-based HIV testing kits compared to 20% in control participants 20% with Risk ratio 2.19 (C.I=1.20-4.01) 36% who requested the test took it and mailed it back compared with 18% in control group . The meta-analysis of the three studies gives Risk ratio of 1.30 with Confidence interval as 1.11-1.53 shows effect estimate as 1.30 times than the comparator group for the studies. I2 of 82.8% shows high heterogeneity. Forest plot for metanalysis is seen in figure 1.
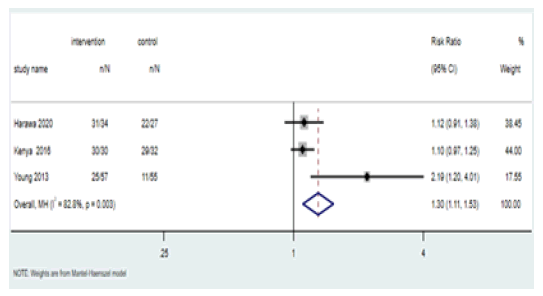
Figure 1: Forest plot for metanalysis
Key: n= number of participants tested for HIV , N = Total number of participants, C.I(Confidence interval), MH(MantelHaenszel)
Exposure to electronic personalized messages recommending matched HIV test vs messages with no recommendation: Frye 2020, recruited 236 young black men and transwomen from online advertising, face to face outreach and participants referrals. Matched as per algorithm questions answered by participants beforehand, they received electronic personalized messages recommending either clinic-based testing or selftesting or Couples HIV Testing and Counselling (CHTC) individually along with resources to find an HIV testing site or CHTC site and control arm messages gave information about each testing method without them completing the questions for the algorithm for a recommended approach and standard HIV information. Electronic personalized messages against messages with no personal recommendation showed very small change in effect on HIV testing with 6 months finding as 73% vs. 72%; p=.81 respectively and R.R of 1.02(C.I=0.87-1.20). HIV testing increased in both arms simultaneously suggesting that an electronic message giving knowledge on available options and/or increasing risk awareness is adequate to remarkably raise HIV testing.
Couple based counselling compared with individual counselling by recruiting 230 AA adult couples from Community Supervision Programs (CSPs) EL, Bassel 2019: Measured primary outcome as various HIV preventive measures and uptake of HIV testing as secondary outcome ,which showed more or less not much change in number of participants who got themselves tested for HIV. Out of 460 participants 341(74.6%) were AA, and results were not mentioned separately but considering larger portion of population as our target population so we included this study. The Power and Connect (PACT) intervention given to couples in experimental arm was guided by social cognitive theory with multiple HIV preventive measures and couple-based skills and control group gave one 45 minute session consisting of individual rapid oral HIV/STI testing with pretest and posttest counseling and referrals to HIV or STI treatment and other social services. PACT intervention group and control group showed 12 months findings as 76/230 (37.6%) and 65/230 (33.9%) respectively with and R.R of 1.17(0.89-1.54).More interventions based on couple-based counselling intervention to increase the uptake of HIV testing as primary outcome could be considered to understand the effect of the same.
The girlfriend project (TGP) party with onsite offer for HIV testing and HIV prevention counselling as an intervention: Hawk et al recruited 149 AA women from community settings through outreach on the street, social environments, civic/ provider groups, and to leaders of subsidized housing communities. TGP facilitator received incentives to host parties for members of their social networks. A single session intervention parties of two hours, where trained facilitators provided HIV risk reduction information, informal assessments and referrals related to addicted and domestic violence and on site HIV oral swab testing compared to the baseline parties conducted to inform women about the study and collect baseline data with no other HIV information shared. Women who reported as HIV negative were only eligible for testing. Out of 49 eligible women from experimental arm 45 women got themselves tested and out of 27 eligible women from control arm, 21 women got themselves tested with R.R of 1.181(C.I=0.95-1.47)
Multi arm intervention-First arm as using provision of free oral swab test, 2nd arm as free mail-in blood sample collection HIV test compared with using medical facility/ community organization of their choice: Merchant 2018 recruited 425 young MSM of different ethnicities of age 18-24 years from multiple social media platforms. Based on criteria of recruitment setting and similarities in intervention implemented, we grouped studies for meta-analysis to observe evidence of effect. The meta-analysis conducted for two different groups of interventions shows R.R as 1.94(C.I-1.50-2.52) in study trials with AA churches as setting showing some effect of evidence and for peer supported intervention R.R was 1.30(C.I=1.11-1.53). Berkley and Derose are pilot study and looking at the effect of this pilot study large population size study is currently under trial(reference) based on the same study design. The intervention based on independent access to HIV testing showed less engagements and more doubts. Peer supported and Church approach are likely to have limited sustainable impact on the uptake of HIV testing. We found no study with Caribbean immigrants as participants. Measures of Implementation process were evaluated only in one study by Derose 2016. The review revealed various types of recruitment settings like AA churches(n=2), community and local venue based(n=5) and multiple settings(n=4), social media platform (n=3) that n Increasing the uptake of HIV testing. High attendance rates and perceived effectiveness were observed in two different grouped studies of peer/CHW supported and AA churches-based studies. Eight studies provided incentives to participants for completing the intervention and one study by Young 2018, did not give incentives. We found 18 studies that met our inclusion criteria, out of which 13 studies are under trial and 5 are said to be complete with no results posted which can be considered potential for any future review. Systematic review by Aung, 2017. identified peer or trained facilitators supported interventions as one of the potential interventions that showed evidence of effect. The population targeted in that review were international immigrants in all countries, so a direct comparison with its findings is not suggestive, owing to difference in challenges of stigma and discrimination, socio-cultural and administrative barriers the immigrants in HICs face. There is no review that is identified targeting the same population and outcome in recent few years .
It was a comprehensive search and addresses a potential research question which is not covered in a systematic review in last few years to our knowledge. Review included only RCTs so other potential non RCT and study designs were refrained to be a part. Screening, data extraction and critical appraisal was conducted was single reviewer leading to few limitations and biases. Time limitation and manpower constraint led to some restrictions in search from grey literature and electronic databases. Findings from studies conducted on MSM population may not be generalized on AA/Caribbean population considering difference in barriers these sub- population faces. All trials included in the review are conducted in US, its applicability in other HICs is conditional due to difference in socio-cultural, economical and structural backgrounds among them. Our inclusion criteria reported exclusively on AA and Caribbean migrants meant that we might have missed interventions from studies that had a broader scope of subject groups such as ethnic minorities.
Though early detection of HIV is identified as instrumental in preventing HIV transmission, very few interventions aiming to increase the HIV testing among AA and Caribbean population in HIC were available through the search. Broader interventions addressing barriers among individual migrant and health care provider, health systems and social determinants at a national level are likely to show evidence of effect. A rigorous grey literature search including contacting authors and organizations operating in this field may provide more evidence of interventions that aim to increase HIV testing uptake among migrants. Researches from various settings, interventions based on more generalized approaches, better service utilization, interventions overcoming stigma, socio-cultural and economical barriers, social determinants of health need to be reviewed to overcome the issue of late HIV testing in the targeted migrant population.
[GoogleScholar] [CrossRef]
Citation: Ritu Chauhan, Plastic Surgery Registrar, Manchester Foundation Trust, United Kingdom. J Pharm Sci Innov. 2023;12(1):http://dx.doi.org/10.7897/2277-4572.114233
Received: 12-Mar-2023, Manuscript No. jpsi-23-92305; Accepted: 18-Jan-2023, Pre QC No. jpsi-23-92305(PQ); Editor assigned: 16-Jan-2023, Pre QC No. jpsi-23-92305(PQ); Reviewed: 17-Jan-2023, QC No. jpsi-23-92305(Q); Revised: 18-Jan-2023, Manuscript No. jpsi-23-92305(R); Published: 20-Jan-2023, DOI: 10.37532/2277-4572.2023.12(1).240
Copyright: This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.